The journey to parenthood is often filled with hope, dreams, and, at times, challenges. For many couples facing infertility, the path can feel overwhelming and uncertain. In this landscape of emotional ups and downs, medical advancements like Intracytoplasmic Sperm Injection (ICSI) offer a beacon of hope.
This revolutionary technique not only enhances the chances of conception but also opens doors to parenthood for countless families around the world.
In recent years, Turkey has emerged as a premier destination for fertility treatments, particularly ICSI. With its cutting-edge technology, highly trained specialists, and a range of world-class clinics, Turkey provides a comprehensive and accessible option for couples seeking effective fertility solutions.
The allure of Turkey doesn’t just lie in its modern medical facilities; it also presents an opportunity for significant cost savings compared to many Western countries.
What is an ICSI procedure?
Intracytoplasmic Sperm Injection (ICSI) is a groundbreaking fertility treatment that has transformed the landscape of assisted reproductive technology (ART).
Designed to tackle various forms of infertility, ICSI is particularly effective for couples facing male-factor infertility, where issues such as low sperm count, poor sperm motility, or abnormal sperm morphology hinder natural conception.
The procedure represents a significant advancement over traditional in vitro fertilization (IVF) methods by allowing clinicians to bypass some of the common barriers to fertilization.
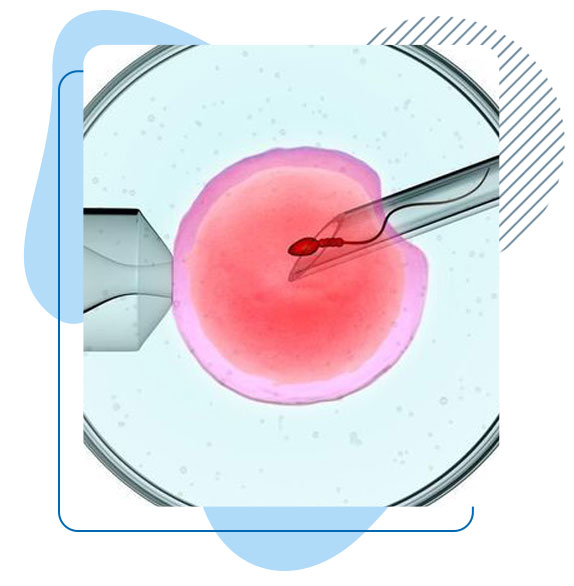
ICSI involves a meticulous process in which a single sperm is selected and directly injected into a mature egg.
This technique dramatically enhances the likelihood of fertilization, especially in scenarios where sperm quality is compromised.
By utilizing ICSI, specialists can significantly increase the chances of successful embryo development and, ultimately, successful pregnancy.
Why undergo an ICSI procedure?
Overcoming Male Factor Infertility
- Directly Addresses Sperm Issues: ICSI is particularly beneficial for couples where male factor infertility is a significant concern. Issues like low sperm count, poor motility, or abnormal sperm shape can hinder natural conception. By injecting a single, viable sperm directly into an egg, ICSI increases the chances of fertilization, even in challenging cases.
Previous IVF Failures
- Improved Success Rates: Couples who have attempted traditional IVF without success may find ICSI to be a more effective alternative. The direct injection of sperm enhances fertilization rates, making it a preferred option for those who have had unsuccessful IVF cycles.
Aging Female Partners
- Maximizing Egg Potential: As women age, their egg quality and quantity tend to decline. ICSI can help maximize the chances of fertilization by ensuring that even eggs from older women can be fertilized effectively, thus improving the likelihood of embryo development.
Genetic Testing of Embryos
- Preimplantation Genetic Diagnosis (PGD): ICSI can facilitate genetic testing of embryos before implantation. This is particularly useful for couples with a known genetic disorder or a family history of genetic conditions. By screening embryos for specific genetic traits, couples can select the healthiest embryos for transfer.
Unexplained Infertility
- Comprehensive Solution: For couples facing unexplained infertility, ICSI can provide a more targeted approach. Since the procedure bypasses many natural barriers to fertilization, it can sometimes lead to successful outcomes even when the underlying cause of infertility remains unidentified.
Low Egg Quality or Quantity
- Enhanced Fertilization: Women with low egg quality or quantity can benefit from ICSI, as the procedure increases the odds of successful fertilization by enabling the use of the best sperm available to fertilize even the least ideal eggs.
Sperm Retrieval Challenges
- Surgical Sperm Collection: In cases where sperm cannot be obtained through ejaculation (e.g., due to certain medical conditions or previous surgeries), ICSI allows for the use of surgically retrieved sperm, making conception possible when traditional methods would fail.
Benefits of ICSI
- Higher Fertilization Rates: ICSI significantly increases the likelihood of fertilization, particularly in cases of male factor infertility where sperm motility or quality may be compromised. By injecting a single sperm directly into an egg, fertilization rates can exceed those of traditional IVF methods.
- Improved Success Rates: Many couples who have experienced unsuccessful IVF cycles find that ICSI enhances their chances of achieving pregnancy. The procedure is often more effective for those with previous failures due to its targeted approach to fertilization.
- Overcoming Specific Infertility Issues: ICSI can address various fertility challenges, such as low sperm count, abnormal sperm morphology, or problems related to egg quality. The direct injection method bypasses many natural barriers that can hinder fertilization.
- Potential for Genetic Testing: ICSI allows for the possibility of preimplantation genetic testing (PGT), enabling the selection of genetically healthy embryos. This is particularly beneficial for couples with a known genetic disorder or those who wish to ensure that their embryos are free from inherited conditions.
- Flexibility with Sperm Sources: The procedure accommodates various sperm retrieval methods, including surgical extraction in cases of azoospermia (absence of sperm in the ejaculate). This flexibility enables couples to use either partner’s sperm or donor sperm.
- Cryopreservation Options: ICSI can lead to the creation of surplus embryos, which can be frozen for future use. This option provides couples with additional chances for pregnancy without the need for repeated ovarian stimulation and egg retrieval cycles.
- Personalized Care and Support: Fertility clinics often provide individualized treatment plans tailored to each couple’s unique situation. This personalized approach enhances the overall patient experience and can contribute to higher success rates.
Risks of ICSI
- Multiple Pregnancies: Similar to IVF, ICSI can lead to the implantation of multiple embryos, increasing the likelihood of multiple pregnancies (twins, triplets, etc.). Multiple pregnancies carry higher risks for both the mother and the babies, including preterm birth and low birth weight.
- Ovarian Hyperstimulation Syndrome (OHSS): Hormonal medications used to stimulate the ovaries can lead to OHSS, a condition characterized by swollen and painful ovaries. In severe cases, it can result in fluid accumulation in the abdomen and chest, requiring medical intervention.
- Invasive Procedures: The ICSI process involves several invasive steps, including egg retrieval and sperm injection. These procedures may carry risks of complications, such as infection, bleeding, or damage to surrounding organs.
- Emotional and Psychological Stress: The fertility treatment process can be emotionally taxing, with high levels of stress, anxiety, and uncertainty. Couples may experience emotional roller coasters throughout the process, particularly with the outcomes of each cycle.
- Potential for Genetic Abnormalities: Although ICSI has been shown to improve fertilization rates, there is some evidence suggesting a slightly increased risk of genetic abnormalities in children conceived through the procedure. This risk is more pronounced for couples with known genetic issues.
- Limited Long-Term Data: While ICSI has been practiced for several decades, long-term studies on the health and development of children conceived via this method are still ongoing. Although most children born through ICSI are healthy, there is still a need for ongoing research.
- Financial Considerations: ICSI can be a costly procedure, with expenses that can quickly add up, especially if multiple cycles are required. While some insurance plans may cover fertility treatments, others may not, leaving couples to navigate the financial burden.
Factors that influence the price of the ICSI procedure in Turkey.
Location of the Clinic
Urban vs. Rural Settings:
- The geographical location of a fertility clinic plays a crucial role in determining the price of ICSI. Clinics located in major urban areas, such as Istanbul, Ankara, and Izmir, often charge higher fees due to the elevated cost of living, real estate prices, and operational expenses in these regions. In contrast, clinics situated in rural or less populous areas may offer more competitive pricing to attract patients.
- The concentration of clinics in urban areas often leads to increased competition, which can influence pricing dynamics. While competition can drive prices down in some cases, well-established clinics with a strong reputation may maintain higher prices due to their perceived quality and success rates.
Reputation and Accreditation:
- The reputation of a clinic is a significant factor in determining its pricing. Clinics that are recognized for their high success rates and positive patient outcomes tend to charge more for their services. Accreditation by international bodies, such as the Joint Commission International (JCI), can also elevate a clinic’s status and result in higher costs, as these clinics adhere to rigorous quality standards and protocols.
- Many patients prioritize choosing a reputable clinic to ensure they receive the best care, and this willingness to invest in quality often results in higher overall costs for treatment.
Experience and Qualifications of the Medical Team
Embryologist Expertise:
- The qualifications and experience of the embryologist performing the ICSI procedure can significantly influence the cost. Highly skilled embryologists with extensive training in reproductive medicine may work in top-tier clinics and typically command higher fees for their services. The level of expertise can directly impact the success rates of the procedure, leading patients to prioritize the skills of the medical team over cost.
- Additionally, clinics that are known for their research and innovative practices may attract leading experts in the field, further driving up costs. Patients seeking the best possible outcomes may find it worthwhile to invest in clinics with renowned specialists.
Doctor’s Credentials:
- The credentials of the fertility specialist overseeing the treatment process also play a crucial role in pricing. Experienced fertility specialists with advanced qualifications, such as board certifications or fellowships in reproductive endocrinology, often charge higher consultation fees. Their depth of knowledge and experience can provide patients with greater confidence in their treatment options and potential outcomes.
- Moreover, specialists with notable success rates in ICSI procedures may establish a reputation that justifies higher fees, as patients are willing to invest in their expertise.
Type of Fertility Treatment Package
Comprehensive Treatment Packages:
- Many clinics offer comprehensive packages that encompass a range of fertility treatments, including hormonal stimulation, egg retrieval, sperm analysis, embryo transfer, and post-treatment follow-up care. These packages can lead to significant savings compared to purchasing each service individually, but they often come with a higher upfront cost.
- It’s important for couples to carefully evaluate what is included in each package. Some clinics may offer all-inclusive options that cover multiple cycles of ICSI, medications, and consultations, while others may have add-ons that increase the overall price.
Additional Services and Testing:
- Beyond the core components of the ICSI procedure, various additional services can contribute to the overall cost. For instance, preimplantation genetic testing (PGT) to screen embryos for genetic conditions can add substantial fees to the treatment. Cryopreservation (freezing) of embryos for future use is another service that can increase costs, as it involves specialized equipment and storage facilities.
- Couples should inquire about the availability of these services and their associated costs when considering ICSI. Understanding the full range of options and any potential additional expenses can aid in budgeting for the entire treatment process.
Laboratory and Technology Costs
Investment in Advanced Technology:
- Clinics that invest in state-of-the-art laboratory equipment and technology often incur higher operational costs. This investment can include advanced imaging systems, automated embryo culture systems, and cryopreservation technologies. Facilities equipped with cutting-edge technology are generally able to provide optimal conditions for fertilization and embryo culture, which can lead to improved success rates.
- While the initial investment in technology can raise prices, patients may find that the enhanced outcomes justify the higher costs, making this an essential consideration when choosing a clinic.
Quality of Materials and Medications:
- The quality of the materials and medications used during the ICSI process can also vary between clinics. Higher-quality medications may lead to better outcomes, as they are often more effective in stimulating ovarian response and improving egg quality. Clinics that prioritize the use of top-tier materials may have higher prices, but this investment can enhance the overall success of the procedure.
- Patients should inquire about the types of medications and protocols used at the clinic to understand how these factors might influence their treatment experience and success rates.
Regulatory Environment and Legal Considerations
National Regulations:
- The regulatory environment surrounding assisted reproductive technologies (ART) in Turkey can impact pricing. Clinics must adhere to various legal requirements, including licensing, quality control measures, and patient safety protocols. Compliance with these regulations can incur additional costs for clinics, which may be passed on to patients through higher fees.
- The Turkish Ministry of Health oversees ART practices, and clinics must meet specific standards to maintain their licenses. As a result, patients should look for clinics that are compliant with national regulations to ensure quality care.
Legal Fees and Documentation:
- In some cases, legal documentation may be required for procedures involving donor sperm or eggs, which can incur additional costs. Patients may need to pay for legal consultations or contracts to protect their rights and responsibilities regarding the use of donor gametes. Understanding these legal aspects can help couples anticipate potential expenses.
Number of Cycles Required
Multiple Treatment Cycles:
- The number of ICSI cycles required to achieve a successful pregnancy can significantly affect the overall cost. While some couples may conceive on their first attempt, others may require multiple cycles, leading to increased expenses. Each cycle typically involves a similar set of costs, including medications, monitoring, and laboratory fees.
- Couples should discuss the potential for multiple cycles with their fertility specialist, as this can help in budgeting and preparing for the financial commitment involved in pursuing ICSI treatment.
Personalized Treatment Plans:
- Some clinics may offer personalized treatment plans that include the possibility of several cycles at a discounted rate. Couples should inquire about these options to better understand the potential for cost savings over the course of their treatment journey.
Patient-Specific Factors
Age and Health History:
- The age and health history of the female partner can influence the treatment plan and costs associated with ICSI. Older women may require more aggressive stimulation protocols or additional tests to assess ovarian reserve, which can increase overall treatment costs.
- Additionally, couples with specific medical conditions may need extra monitoring, medications, or interventions, leading to higher expenses. Understanding these individual factors can help couples anticipate potential costs and discuss personalized options with their fertility specialist.
Sperm Quality and Source:
- The quality of the sperm used in the ICSI procedure can also influence costs. In cases of male factor infertility, where sperm quality is compromised, additional procedures, such as testicular sperm extraction (TESE) or sperm washing, may be necessary, adding to the overall price.
- Couples opting for donor sperm may also encounter additional fees for screening and procurement, further impacting the total cost of the procedure.
Insurance Coverage and Financial Assistance
Insurance Plans:
- The level of insurance coverage for fertility treatments can significantly influence out-of-pocket expenses. Some insurance plans may cover a portion of the costs associated with ICSI, while others may not provide coverage at all. Patients should thoroughly review their insurance policies and discuss coverage options with their providers to understand potential financial obligations.
- In Turkey, some public and private insurance plans offer coverage for specific fertility treatments, which can alleviate the financial burden for eligible couples. It’s essential for patients to check their insurance status to see what is covered.
Payment Plans and Financing Options:
- Many clinics offer flexible payment plans or financing options to help couples manage the costs of ICSI. This may include installment payment plans or partnerships with financial institutions that specialize in healthcare financing. Patients should inquire about these options to find a solution that fits their financial situation.
- Understanding the availability of financial assistance can empower couples to pursue the treatments they need without facing overwhelming financial strain.
Prices of all types of the ICSI procedure in Turkey.
Conventional ICSI (Intracytoplasmic Sperm Injection)
Definition and Details:
Conventional ICSI is a widely used procedure to address male infertility by directly injecting a single sperm into a mature egg.
This technique is highly effective for couples struggling with conditions such as low sperm count, poor sperm motility, or abnormal sperm shape, which often prevent sperm from naturally penetrating the egg.
The process begins with ovarian stimulation, where the female partner takes hormonal injections to stimulate the ovaries to produce multiple eggs.
Once the eggs have matured, they are retrieved via a minor surgical procedure and injected with sperm in a laboratory.
Procedure Steps:
- Initial Consultation and Fertility Evaluation: A comprehensive examination of the couple’s fertility health, including semen analysis and ovarian reserve tests.
- Ovarian Stimulation: The female partner takes hormone injections to stimulate the ovaries to produce multiple eggs.
- Monitoring with Ultrasound and Blood Tests: The development of eggs is tracked using ultrasounds and blood tests to determine when they are ready for retrieval.
- Egg Retrieval: Mature eggs are retrieved in a short procedure using a needle guided by ultrasound, performed under light sedation.
- Sperm Collection: The male partner provides a fresh semen sample or undergoes surgical sperm retrieval if necessary.
- ICSI Procedure: A single sperm is injected into each mature egg under a microscope by an experienced embryologist.
- Embryo Culture: The fertilized eggs are monitored as they develop into embryos in a specialized laboratory.
- Embryo Transfer: The healthiest embryos are selected and transferred into the uterus to initiate pregnancy.
- Luteal Support: Hormonal supplements are prescribed to support embryo implantation and early pregnancy.
- Pregnancy Test: A blood test is performed two weeks after the embryo transfer to confirm pregnancy.
Pricing Breakdown:
- Initial Consultation and Fertility Evaluation: $150 – $300
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- Sperm Collection (Natural): $100 – $300
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for Conventional ICSI: $5,500 – $13,900
ICSI with Assisted Hatching (AH)
Definition and Details:
ICSI with Assisted Hatching is an advanced technique that combines traditional ICSI with an additional step known as assisted hatching.
In some cases, embryos may have a thicker outer shell (zona pellucida), which makes it difficult for the embryo to “hatch” and implant into the uterine wall.
To help the embryo break free from its shell, assisted hatching is performed by creating a small opening in the zona pellucida using a laser, chemical, or mechanical method.
This technique is especially beneficial for patients with multiple failed IVF cycles, women over the age of 37, or those using frozen embryos, which may develop a hardened zona after the freezing process. Laser-assisted hatching is the most precise method, allowing for better embryo implantation without risking damage to the embryo.
By enhancing the embryo’s ability to implant, this procedure improves the likelihood of pregnancy for patients with challenging fertility conditions.
Procedure Steps:
- Initial Consultation and Fertility Evaluation: The couple undergoes fertility testing to determine if assisted hatching is necessary.
- Ovarian Stimulation: Hormonal injections are given to the female partner to stimulate egg production.
- Monitoring of Egg Development: Ultrasounds and blood tests are used to track the development of eggs.
- Egg Retrieval Procedure: Eggs are collected from the ovaries using a needle and ultrasound guidance, under sedation.
- Sperm Collection: A sperm sample is provided by the male partner, or sperm is surgically retrieved if needed.
- ICSI Procedure: A single sperm is injected into each egg in the laboratory.
- Embryo Culture: The fertilized eggs develop into embryos in a controlled lab environment.
- Assisted Hatching Procedure: A small hole is made in the outer shell of the embryos to assist in implantation.
- Embryo Transfer: The best-quality embryo(s) is selected for transfer into the uterus.
- Luteal Support: Hormonal supplements are given to support early pregnancy.
- Pregnancy Test: Two weeks post-transfer, a pregnancy test is conducted to check for pregnancy.
Pricing Breakdown:
- Initial Consultation and Fertility Evaluation: $150 – $300
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- Sperm Collection (Natural): $100 – $300
- Sperm Collection (Surgical): $1,500 – $3,000
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Laser-Assisted Hatching: $500 – $1,000
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Assisted Hatching: $6,000 – $15,400
ICSI with Preimplantation Genetic Testing (PGT-A)
Definition and Details:
ICSI with Preimplantation Genetic Testing for Aneuploidies (PGT-A) is an advanced reproductive technique that adds a layer of genetic testing to the ICSI process. In this procedure, after the sperm is injected into the egg and the embryos develop to the blastocyst stage (5-6 days), a few cells are biopsied from the outer layer of the embryo.
These cells are then sent for genetic testing to detect chromosomal abnormalities such as Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and other aneuploidies that may affect the viability of the embryo or the health of the baby.
This type of ICSI is particularly recommended for older women (typically over the age of 37), couples who have experienced recurrent miscarriages, and those with a history of failed IVF cycles. It is also useful for couples with known genetic conditions, as it allows for the selection of embryos that are free from specific chromosomal disorders.
By ensuring that only chromosomally normal embryos are transferred, PGT-A significantly improves the chances of a successful pregnancy and reduces the risk of miscarriage.
Procedure Steps:
- Initial Consultation and Genetic Counseling: A detailed consultation to evaluate the need for genetic testing and counsel couples on the benefits of PGT-A.
- Ovarian Stimulation: Hormonal injections to stimulate the female partner’s ovaries to produce multiple eggs.
- Monitoring of Egg Development: Ultrasound scans and blood tests to track egg growth and determine the best time for retrieval.
- Egg Retrieval Procedure: The eggs are collected from the ovaries using a minimally invasive procedure.
- Sperm Collection: The male partner provides a fresh sperm sample, or sperm is surgically retrieved if needed.
- ICSI Procedure: Sperm is injected into each egg by the embryologist in the lab.
- Embryo Culture: The fertilized eggs develop into embryos under controlled laboratory conditions.
- Embryo Biopsy for Genetic Testing: A few cells are removed from the outer layer of the embryo for genetic analysis.
- PGT-A Testing: The biopsied cells are sent for genetic testing to screen for chromosomal abnormalities.
- Embryo Transfer: Chromosomally normal embryos are selected and transferred into the uterus.
- Luteal Support: Hormonal support is provided to help the embryo implant and sustain early pregnancy.
- Pregnancy Test: A blood test is conducted after two weeks to confirm pregnancy.
Pricing Breakdown:
- Initial Consultation and Genetic Counseling: $200 – $400
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- Sperm Collection (Natural): $100 – $300
- Sperm Collection (Surgical): $1,500 – $3,000
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Biopsy for Genetic Testing: $1,500 – $2,500
- PGT-A Genetic Testing: $3,000 – $5,000
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with PGT-A: $10,400 – $22,800
ICSI with Surgical Sperm Retrieval (TESE/MESA)
Definition and Details:
ICSI with Surgical Sperm Retrieval involves the combination of ICSI with specialized techniques to extract sperm directly from the male reproductive system when ejaculation is not possible or when there is a lack of sperm in the ejaculate (azoospermia).
This procedure is beneficial for men who face severe male infertility, including obstructive azoospermia (where a blockage prevents sperm from appearing in the ejaculate) or non-obstructive azoospermia (where the testes are unable to produce sperm naturally).
Two common methods of sperm retrieval are Testicular Sperm Extraction (TESE) and Microsurgical Epididymal Sperm Aspiration (MESA).
TESE involves a minor surgical procedure to extract sperm directly from the testes, while MESA retrieves sperm from the epididymis. Once sperm is extracted, it is immediately injected into the eggs via ICSI to enable fertilization.
The procedure offers hope to men who would otherwise have no chance of biologically fathering a child, making it a crucial tool for treating severe male factor infertility.
Procedure Steps:
- Initial Consultation and Male Fertility Assessment: An evaluation of the male partner’s fertility, including tests to determine sperm presence and quality.
- Ovarian Stimulation for Female Partner: Hormonal injections to stimulate the female partner’s ovaries to produce eggs.
- Monitoring of Egg Development: Regular ultrasounds and blood tests to track ovarian response.
- Surgical Sperm Retrieval (TESE or MESA): Sperm is surgically extracted from the testes (TESE) or epididymis (MESA) under local or general anesthesia.
- Sperm Analysis and Preparation: Extracted sperm is examined and prepared for injection into the eggs.
- ICSI Procedure: A single sperm is injected into each mature egg.
- Embryo Culture: The fertilized eggs develop into embryos in a controlled lab environment.
- Embryo Transfer: The best-quality embryos are selected and transferred into the uterus.
- Luteal Support: Hormonal medications are provided to support implantation and early pregnancy.
- Pregnancy Test: Two weeks after the embryo transfer, a blood test is done to confirm pregnancy.
Pricing Breakdown:
- Initial Consultation and Male Fertility Assessment: $200 – $400
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Surgical Sperm Retrieval (TESE/MESA): $2,500 – $5,000
- Sperm Analysis and Preparation: $300 – $500
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Surgical Sperm Retrieval: $7,000 – $15,500
ICSI with Frozen Embryo Transfer (FET)
Definition and Details:
ICSI with Frozen Embryo Transfer (FET) involves using embryos that were previously created and frozen for future use.
This procedure is often selected by couples who have undergone a prior IVF or ICSI cycle and have had excess embryos cryopreserved (frozen) for later attempts. FET is also ideal for patients who wish to avoid the physical and financial burdens of undergoing ovarian stimulation and egg retrieval again, as the embryos are already available.
Frozen embryos can be thawed and transferred to the uterus during the natural or a hormonally prepared cycle.
FET is also beneficial for patients who wish to undergo genetic testing on embryos prior to transfer, as the embryos can be biopsied and frozen while awaiting test results. Frozen embryos are equally viable as fresh ones, and in some cases, they have even shown slightly higher success rates due to the ability to better time the uterus preparation and embryo transfer process.
Procedure Steps:
- Initial Consultation and Embryo Evaluation: Review of previously frozen embryos to determine their quality and suitability for transfer.
- Preparation of the Uterus: Hormonal medications (estrogen and progesterone) are used to prepare the uterine lining for embryo transfer.
- Thawing of Frozen Embryos: The cryopreserved embryos are carefully thawed in a lab environment to ensure they survive the process.
- Embryo Transfer: Once thawed, the best-quality embryo is transferred into the uterus using a thin catheter.
- Luteal Support: Hormonal support is given post-transfer to help implantation.
- Pregnancy Test: A pregnancy test is performed after two weeks to check for successful implantation.
Pricing Breakdown:
- Initial Consultation and Embryo Evaluation: $200 – $400
- Preparation of the Uterus (Hormonal Medications): $300 – $600
- Thawing of Frozen Embryos: $500 – $800
- Embryo Transfer Procedure: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Frozen Embryo Transfer (FET): $1,800 – $3,600
ICSI with Egg Donation
Definition and Details:
ICSI with Egg Donation is a specialized procedure in which a donor’s eggs are used instead of the intended mother’s eggs to achieve pregnancy.
This method is recommended for women who are unable to produce healthy eggs, typically due to advanced age, poor ovarian reserve, or other medical conditions.
In this procedure, the donor undergoes ovarian stimulation and egg retrieval, and the collected eggs are then fertilized with the male partner’s sperm using ICSI.
The resulting embryos are cultured and then transferred into the intended mother’s uterus. The process allows couples facing female infertility to have a biological child with the male partner’s genetics.
Egg donation programs in Turkey follow stringent protocols to ensure that donors are thoroughly screened for genetic and infectious diseases. Donor anonymity is typically maintained, but detailed profiles regarding the donor’s physical characteristics, education, and health background are available to assist with the selection process.
Procedure Steps:
- Initial Consultation and Donor Selection: Selection of a suitable egg donor after thorough medical and genetic screening.
- Ovarian Stimulation of Egg Donor: Hormonal injections are administered to the donor to stimulate egg production.
- Monitoring of Donor’s Egg Development: Ultrasounds and blood tests are performed to track the donor’s ovarian response.
- Egg Retrieval from Donor: Mature eggs are collected from the donor via a minimally invasive procedure.
- Sperm Collection from Male Partner: The male partner provides a semen sample or undergoes surgical sperm retrieval if necessary.
- ICSI Procedure: The donor’s eggs are injected with sperm from the male partner using ICSI.
- Embryo Culture: Fertilized eggs are cultured into embryos under controlled laboratory conditions.
- Embryo Transfer: The healthiest embryo(s) is transferred into the intended mother’s uterus.
- Luteal Support: Hormonal medications are provided to support the uterine lining and help the embryo implant.
- Pregnancy Test: A blood test is conducted two weeks post-transfer to confirm pregnancy.
Pricing Breakdown:
- Initial Consultation and Donor Selection: $500 – $1,000
- Ovarian Stimulation of Egg Donor: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests (Donor): $500 – $800
- Egg Retrieval Procedure (Donor): $800 – $1,500
- Sperm Collection from Male Partner: $100 – $300
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Transfer into Intended Mother: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Egg Donation: $7,400 – $15,400
ICSI with Sperm Donation
Definition and Details:
ICSI with Sperm Donation is a procedure where donor sperm is used to fertilize the eggs of the female partner, typically through ICSI.
This method is recommended for couples where the male partner is unable to produce viable sperm due to genetic disorders, azoospermia, or other fertility issues.
In some cases, couples may choose sperm donation when there is a high risk of passing genetic conditions to offspring. Donor sperm can be sourced from accredited sperm banks, where donors are thoroughly screened for genetic, infectious, and health-related factors.
After sperm is selected, it is thawed and used in the ICSI process, where it is injected directly into the eggs.
The resulting embryos are then cultured and transferred to the female partner’s uterus. Sperm donors are often anonymous, but couples can review profiles that include information about the donor’s background, physical traits, and health.
Procedure Steps:
- Initial Consultation and Donor Selection: The sperm donor is chosen based on genetic screening and personal preferences.
- Ovarian Stimulation for Female Partner: The female partner undergoes hormonal treatment to stimulate the production of multiple eggs.
- Monitoring of Egg Development: Ultrasounds and blood tests monitor the ovaries’ response to stimulation.
- Egg Retrieval from Female Partner: Mature eggs are retrieved from the ovaries in a minor surgical procedure.
- Thawing and Preparation of Donor Sperm: The selected donor sperm is thawed and prepared for injection.
- ICSI Procedure: A single sperm is injected into each egg using the ICSI method.
- Embryo Culture: The fertilized eggs are cultured in a lab until they become embryos.
- Embryo Transfer: The best embryos are selected for transfer into the female partner’s uterus.
- Luteal Support: Hormonal medications are provided to support implantation.
- Pregnancy Test: Two weeks after the embryo transfer, a pregnancy test is performed.
Pricing Breakdown:
- Initial Consultation and Donor Selection: $500 – $1,000
- Ovarian Stimulation Medications for Female Partner: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- Thawing and Preparation of Donor Sperm: $300 – $600
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Sperm Donation: $6,600 – $12,700
ICSI with Pre-Implantation Genetic Diagnosis (PGD)
Definition and Details:
ICSI with Pre-Implantation Genetic Diagnosis (PGD) is a sophisticated reproductive technology designed to screen embryos for genetic disorders before implantation.
This method is typically recommended for couples who are at high risk of passing on serious genetic diseases, such as cystic fibrosis, thalassemia, or muscular dystrophy, to their offspring. PGD can also be used by couples who have experienced repeated miscarriages or failed IVF cycles, as it helps ensure the healthiest embryos are selected for transfer.
In this procedure, the eggs are fertilized using ICSI, and once the embryos reach the blastocyst stage (typically on day 5), a small biopsy is performed to extract a few cells from each embryo for genetic testing.
The embryos are then analyzed for chromosomal abnormalities or specific genetic mutations. Only genetically healthy embryos are selected for transfer to the uterus, reducing the risk of inherited genetic disorders and improving the likelihood of a successful pregnancy. The remaining embryos that pass the genetic screening can be frozen for future use.
Procedure Steps:
- Initial Consultation and Genetic Counseling: The couple meets with a genetic counselor to assess their risk factors and discuss the need for PGD.
- Ovarian Stimulation for Female Partner: Hormonal medications are administered to stimulate the production of multiple eggs.
- Monitoring of Egg Development: Regular ultrasounds and blood tests track the ovarian response to stimulation.
- Egg Retrieval Procedure: The mature eggs are retrieved from the ovaries through a minor surgical procedure.
- ICSI Procedure: Sperm is injected into each egg to achieve fertilization.
- Embryo Culture: Fertilized eggs are cultured into embryos in a controlled lab environment.
- Embryo Biopsy: A few cells are carefully extracted from each embryo for genetic testing.
- Genetic Analysis: The biopsied cells are tested for chromosomal abnormalities or specific genetic disorders.
- Embryo Selection: Only healthy embryos free from genetic issues are selected for transfer.
- Embryo Transfer: The healthiest embryo(s) is transferred into the uterus.
- Luteal Support: Hormonal medications are provided to support the implantation process.
- Pregnancy Test: A pregnancy test is conducted two weeks after the embryo transfer.
Pricing Breakdown:
- Initial Consultation and Genetic Counseling: $300 – $500
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Biopsy: $1,500 – $3,000
- Genetic Analysis: $3,000 – $5,000
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Pre-Implantation Genetic Diagnosis (PGD): $10,600 – $19,600
ICSI with Pre-Implantation Genetic Screening (PGS)
Definition and Details:
ICSI with Pre-Implantation Genetic Screening (PGS) is a method used to screen embryos for chromosomal abnormalities before they are implanted into the uterus.
Unlike PGD, which tests for specific genetic disorders, PGS is used to check for general chromosomal abnormalities, such as Down syndrome, Turner syndrome, or other aneuploidies.
This technique is especially beneficial for older women (over the age of 35), women who have experienced recurrent miscarriages, or couples who have had unsuccessful IVF cycles. By ensuring that only chromosomally normal embryos are transferred, PGS increases the likelihood of a successful pregnancy and reduces the risk of miscarriage.
Similar to PGD, PGS involves performing a biopsy on the embryos at the blastocyst stage, and the cells are tested for chromosomal abnormalities. Only embryos with the correct number of chromosomes are selected for transfer.
The remaining embryos can be frozen for future use. This method ensures that the embryos with the highest chance of leading to a healthy pregnancy are used, maximizing success rates.
Procedure Steps:
- Initial Consultation and Screening: The couple undergoes an evaluation to determine their eligibility for PGS.
- Ovarian Stimulation for Female Partner: Hormonal injections are administered to stimulate the ovaries to produce multiple eggs.
- Monitoring of Egg Development: Ultrasounds and blood tests monitor the growth of the ovarian follicles.
- Egg Retrieval Procedure: The mature eggs are collected through a minor surgical procedure.
- ICSI Procedure: Each egg is fertilized using ICSI.
- Embryo Culture: The embryos are cultured in a lab for several days until they reach the blastocyst stage.
- Embryo Biopsy: A small number of cells are removed from the blastocyst for chromosomal analysis.
- Genetic Screening: The biopsied cells are analyzed for chromosomal abnormalities.
- Embryo Selection: Only chromosomally normal embryos are selected for transfer.
- Embryo Transfer: The selected embryo is transferred to the uterus.
- Luteal Support: Hormonal medications are provided to support implantation.
- Pregnancy Test: A pregnancy test is performed two weeks after embryo transfer to confirm the success of the procedure.
Pricing Breakdown:
- Initial Consultation and Screening: $200 – $500
- Ovarian Stimulation Medications: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Embryo Biopsy: $1,500 – $3,000
- Genetic Screening (PGS): $3,000 – $5,000
- Embryo Transfer: $500 – $1,000
- Luteal Support Medications: $200 – $500
- Pregnancy Test and Follow-up: $100 – $300
- Total Estimated Cost for ICSI with Pre-Implantation Genetic Screening (PGS): $10,500 – $19,600
ICSI with Surrogacy
Definition and Details:
ICSI with Surrogacy is a reproductive option where a surrogate mother carries and delivers a child for another couple.
This procedure is recommended when the intended mother cannot carry a pregnancy due to health reasons, such as uterine abnormalities, previous hysterectomy, or other medical conditions that make pregnancy unsafe.
In this process, the eggs from the intended mother (or an egg donor) are fertilized using ICSI, and the resulting embryos are transferred into the surrogate’s uterus.
Surrogacy is a complex arrangement that requires legal, medical, and psychological consultations to ensure that both the intended parents and the surrogate fully understand the process. The surrogate carries the pregnancy to term, and the intended parents assume legal guardianship of the child upon birth.
In many cases, surrogacy involves additional legal costs to ensure that the parental rights of the intended parents are protected.
Procedure Steps:
- Initial Consultation and Surrogate Matching: The couple selects a surrogate mother, and legal agreements are arranged.
- Ovarian Stimulation for Female Partner or Egg Donor: The intended mother or egg donor undergoes hormonal treatment to produce multiple eggs.
- Monitoring of Egg Development: Ultrasounds and blood tests monitor the growth of the ovarian follicles.
- Egg Retrieval Procedure: Mature eggs are collected from the ovaries.
- ICSI Procedure: Sperm from the intended father is injected into the retrieved eggs.
- Embryo Culture: The fertilized eggs are cultured into embryos in a lab.
- Preparation of the Surrogate’s Uterus: The surrogate receives hormonal treatment to prepare her uterus for embryo implantation.
- Embryo Transfer: The best-quality embryo(s) is transferred into the surrogate’s uterus.
- Luteal Support for Surrogate: The surrogate receives hormonal support to ensure the success of the implantation.
- Pregnancy and Birth: The surrogate carries the pregnancy to term, and the intended parents receive legal guardianship of the baby upon delivery.
Pricing Breakdown:
- Initial Consultation and Surrogate Matching: $5,000 – $10,000
- Ovarian Stimulation Medications for Intended Mother/Egg Donor: $1,200 – $3,000
- Monitoring with Ultrasound and Blood Tests: $500 – $800
- Egg Retrieval Procedure: $800 – $1,500
- ICSI Procedure: $1,500 – $2,500
- Embryo Culture: $1,000 – $1,500
- Preparation of Surrogate’s Uterus: $500 – $1,000
- Embryo Transfer to Surrogate: $500 – $1,000
- Luteal Support for Surrogate: $200 – $500
- Legal and Surrogacy Fees: $15,000 – $50,000
- Total Estimated Cost for ICSI with Surrogacy: $26,200 – $70,800
What happens during an ICSI procedure?
Oocyte Retrieval (Egg Collection)
Overview: The first step involves retrieving mature eggs from the ovaries using a minor surgical procedure known as transvaginal ultrasound aspiration. This procedure is typically performed under sedation or anesthesia to ensure comfort.
Doctor’s Actions:
- Preparation: The doctor ensures the patient is comfortable and monitors vital signs during the procedure.
- Ultrasound Guidance: Utilizing an ultrasound machine, the doctor locates the follicles containing mature eggs.
- Needle Aspiration: A thin, hollow needle is carefully inserted through the vaginal wall and into each follicle to retrieve the eggs, which are then suctioned out.
- Assessment: The retrieved eggs are examined under a microscope to confirm their maturity.
Sperm Collection
Overview: While the eggs are being retrieved, sperm is collected from the male partner or a sperm donor.
If there are issues with sperm production or quality, the doctor may opt for sperm retrieval techniques.
Doctor’s Actions:
- Semen Analysis: The doctor analyzes the sperm sample for count, motility, and morphology to select the healthiest sperm.
- Sperm Processing: The doctor processes the semen sample using a centrifuge to separate the sperm from seminal fluid and enhance concentration.
- Sperm Selection: A selection is made for the most viable sperm for injection, potentially using a technique like ICSI or, if necessary, sperm retrieval techniques such as testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA).
Sperm Injection into Oocytes
Overview: In this pivotal step, a single healthy sperm is injected directly into a mature egg using a micromanipulation technique. This process ensures that even sperm with motility issues can achieve fertilization.
Doctor’s Actions:
- Micromanipulator Setup: The doctor prepares a micromanipulator system, which allows for precise handling of both the sperm and the egg.
- Sperm Immobilization: The selected sperm is immobilized using a fine glass pipette, preventing any movement during the injection.
- Injection Procedure: The doctor carefully positions the egg under a microscope and uses a second pipette to inject the sperm directly into the cytoplasm of the egg.
- Monitoring: The doctor closely observes the egg to ensure successful sperm injection and minimizes any potential damage.
Fertilization Monitoring
Overview: Following sperm injection, the fertilized eggs (now called zygotes) are monitored for signs of fertilization over the next 16-20 hours.
Doctor’s Actions:
- Incubator Placement: The fertilized eggs are placed in a specialized incubator that maintains optimal conditions for growth and development.
- Microscopic Observation: The doctor examines the eggs under a microscope at regular intervals to check for signs of fertilization, such as the presence of two pronuclei.
- Documentation: Each zygote’s progress is documented meticulously to track which ones successfully fertilized.
Embryo Culture
Overview: After successful fertilization, the zygotes are cultured to develop into embryos. The embryo culture phase lasts typically between 3 to 5 days, depending on the clinic’s protocol and the embryos’ development.
Doctor’s Actions:
- Embryo Transfer Preparation: The doctor prepares to transfer the healthiest embryos by monitoring their growth closely and selecting the optimal number for transfer based on quality.
- Media Changes: The culture media may be refreshed to provide nutrients and facilitate optimal growth.
- Assessment: Daily assessments are conducted to evaluate the embryos’ developmental stage, morphology, and overall health.
Embryo Selection for Transfer
Overview: Once the embryos have developed, the doctor selects the best quality embryos for transfer. Typically, only one or two embryos are chosen to minimize the risk of multiple pregnancies.
Doctor’s Actions:
- Morphological Evaluation: The doctor examines the embryos’ size, shape, and cell division rate to assess their quality.
- Grading System: Embryos are graded based on established criteria, such as the number of cells and uniformity of cell size, to determine their viability.
- Consultation with the Patient: The doctor discusses the embryo selection process with the patient(s) and makes recommendations based on the quality and the patient’s preferences.
Embryo Transfer Procedure
Overview: The selected embryos are transferred into the uterus through a thin catheter. This procedure is usually painless and done in a sterile environment.
Doctor’s Actions:
- Preparation of the Uterus: The doctor may use ultrasound to ensure the bladder is full, which helps visualize the uterus.
- Catheter Insertion: The doctor carefully inserts a soft catheter into the uterus, ensuring it’s positioned correctly to avoid any discomfort.
- Embryo Placement: Using a syringe attached to the catheter, the doctor gently releases the selected embryos into the uterine cavity.
- Observation: The doctor monitors the transfer process to ensure it goes smoothly, checking for any complications.
Post-Transfer Care
Overview: After the embryo transfer, the patient will be monitored for a brief period before being allowed to return home.
Doctor’s Actions:
- Post-Procedure Observation: The doctor observes the patient for a short time to ensure there are no immediate complications from the procedure.
- Instructions for Care: The doctor provides guidance on post-transfer care, including medications and lifestyle modifications to enhance implantation chances.
- Follow-Up Schedule: A follow-up appointment is arranged for pregnancy testing and further monitoring.
Cryopreservation of Extra Embryos
Overview: If there are viable embryos remaining after the transfer, they may be frozen for future use. This allows couples to attempt pregnancy again without undergoing the full ICSI process.
Doctor’s Actions:
- Embryo Evaluation: The doctor assesses the remaining embryos for their viability before freezing.
- Freezing Process: A cryoprotectant is applied, and the embryos are gradually cooled to prevent ice crystal formation, then stored in liquid nitrogen.
- Documentation: Each frozen embryo is carefully labeled and documented for future reference.
Pregnancy Test and Monitoring
Overview: Approximately 10-14 days after the embryo transfer, a blood test is performed to determine if the procedure was successful.
Doctor’s Actions:
- Blood Sample Collection: The doctor arranges for a blood draw to measure levels of human chorionic gonadotropin (hCG), indicating pregnancy.
- Interpreting Results: The doctor interprets the results and informs the patient of the outcome, discussing next steps based on whether the pregnancy is confirmed or not.
What happens after an ICSI procedure?
Short-Term Healing Period (Days 1-7)
The initial days after the ICSI procedure are vital for ensuring optimal recovery and preparing the body for implantation.
Immediate Recovery
- Observation: After the embryo transfer, patients typically remain in the clinic for a brief observation period, usually lasting around 30 minutes to an hour. During this time, medical staff monitor vital signs and assess any immediate discomfort.
- Rest: Patients are encouraged to rest, both physically and emotionally. Although the embryo transfer is generally not physically painful, some may experience mild cramping or discomfort similar to menstrual cramps.
Managing Symptoms
- Pain Management: Over-the-counter pain relief medications like acetaminophen may be recommended to manage any discomfort. Patients should avoid non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen unless specifically instructed by their doctor.
- Hydration and Nutrition: Staying hydrated and maintaining a healthy diet rich in vitamins and minerals is important. Foods high in antioxidants, such as fruits and vegetables, are especially beneficial during this period.
Activity Restrictions
- Avoiding Strenuous Activity: Patients are advised to refrain from intense physical activities, such as heavy lifting, strenuous exercise, or sexual intercourse, for at least a week after the procedure. This minimizes the risk of complications and promotes a supportive environment for embryo implantation.
- Light Activities: Gentle walking and light activities can be beneficial to promote circulation and prevent stiffness. However, these should be done with caution and under the guidance of a healthcare provider.
Medications
- Hormonal Support: Following the ICSI procedure, patients are often prescribed hormonal medications, such as progesterone supplements, to support the uterine lining and enhance the chances of embryo implantation. Patients should adhere to the prescribed regimen and report any adverse effects to their doctor.
- Fertility Drugs: If applicable, the doctor may continue to prescribe fertility medications during this period to regulate hormones and encourage a conducive environment for pregnancy.
Long-Term Healing Period (Weeks 1-12)
As the weeks progress after the ICSI procedure, the focus shifts from immediate recovery to monitoring for potential pregnancy and overall well-being.
Emotional Well-being
- Support System: The emotional aspect of this period is significant, as it can be filled with anxiety and uncertainty. Engaging with a support system whether family, friends, or support groups can provide comfort and encouragement during this waiting period.
- Mental Health Resources: Patients are encouraged to seek counseling or join support groups for couples undergoing fertility treatments. Mental health professionals can provide coping strategies for dealing with stress, anxiety, and any emotional challenges that arise.
Monitoring for Pregnancy
- Pregnancy Test: Approximately 10-14 days after the embryo transfer, a blood test will be conducted to check for the presence of hCG, a hormone indicating pregnancy. The results will guide the next steps, including continued monitoring and care.
- Follow-Up Appointments: If pregnancy is confirmed, the doctor will schedule follow-up appointments to monitor the pregnancy’s progress, usually starting around 4-6 weeks after the procedure.
Physical Health Maintenance
- Continued Medications: Patients may continue taking hormonal support medications during the early weeks of pregnancy, as prescribed by the doctor. Adhering to this regimen is crucial for maintaining a healthy pregnancy.
- Lifestyle Adjustments: Healthy lifestyle choices should be maintained throughout this period. Patients are advised to avoid smoking, limit caffeine intake, and abstain from alcohol and recreational drugs to create a healthy environment for the developing embryo.
Recognizing Signs of Complications
- Potential Symptoms: Patients should be vigilant for any unusual symptoms such as severe abdominal pain, heavy bleeding, or signs of infection (fever, chills). These symptoms should be reported to a healthcare provider immediately.
- Ectopic Pregnancy: In rare cases, an ectopic pregnancy may occur, where the embryo implants outside the uterus. Symptoms may include severe abdominal pain on one side, vaginal bleeding, or shoulder pain. Prompt medical evaluation is essential if these symptoms arise.
Preparing for Follow-Up Care
- Continued Medical Oversight: After the initial pregnancy test, regular monitoring will be necessary to track hormone levels and ensure the health of the pregnancy. This may involve blood tests and ultrasound examinations to assess fetal development.
- Planning for Future Steps: Depending on the outcome of the pregnancy test and subsequent appointments, discussions with the doctor about potential next steps will be necessary. This may include considerations for further monitoring, lifestyle changes, or additional fertility treatments if pregnancy does not occur.
Conclusion.
The journey to parenthood through ICSI can be a daunting yet rewarding experience. Understanding the complete cost structure involved allows couples to plan better and make informed decisions about their fertility options.
Turkey offers a compelling blend of affordable prices, skilled medical professionals, and high success rates, making it a top choice for couples looking to conceive.
As you embark on this journey, always consult with qualified fertility specialists who can guide you through the process, providing tailored recommendations that suit your needs.
